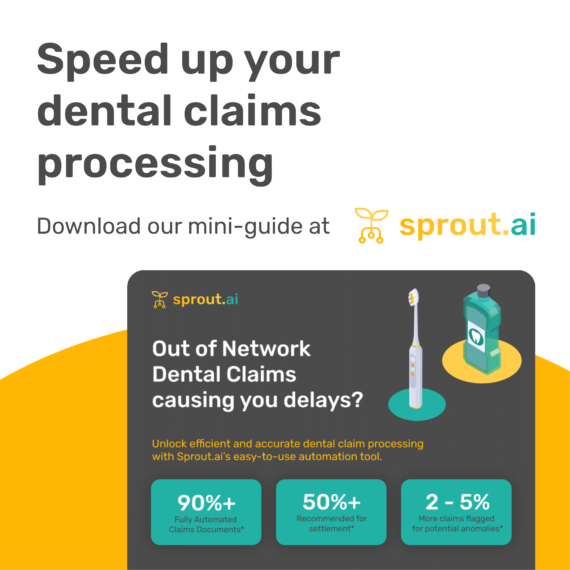
Missing information, unstructured evidence and document overload delaying dental claims? Here’s how Sprout.ai can help
If you’re looking to boost the efficiency of your out-of-network dental claims processing and provide a seamless experience for your customers, we’re here to help.
Sprout.ai enables:
- Improved efficiency
- Fewer errors
- Faster claim processing
- Enhanced fraud detection
Here’s how Sprout.ai works
Extraction and identification of key information
Sprout.ai can extract and identify essential information from unstructured dental documents. This includes patient information, treatment details, dates, and more. By automating this process, Sprout.ai eliminates the need for manual data entry, reducing the chances of errors and speeding up the claims process.
Validation and contextualisation
Once the information is extracted, Sprout.ai goes a step further by validating and contextualising it. This means that the extracted data is not just presented as raw text but is structured and organised in a way that makes sense for internal dental claims systems. This includes codifying treatment line items, making it easier for claims handlers to review and process the information.
Automated checks and claims handling logic
Sprout.ai also performs automated checks and applies claims handling logic to ensure accuracy and consistency. The checks and validations include:
- Duplicate document and tampering checks to prevent fraud.
- Flagging inflated treatment costs to safeguard against overbilling.
- Detecting proximity anomalies that may indicate errors or inconsistencies.
- Identifying treatment inconsistencies to ensure that claims align with standard procedures.
Interested in learning more about enhancing out-of-network dental claim processing? Download our mini guide to out-of-network dental claims.