In our research report, Customer Experience: The Claim Handler’s Perspective, we asked life insurance claims handlers about their daily challenges, factors delaying processing, and customer needs.
We found that life insurance claims involve unique challenges such as high levels of customer support, complex documentation, and lengthy approval processes. With the right tools, these challenges can be addressed, leading to more efficient operations, improved customer satisfaction, and a more fulfilled workforce.
The unique challenges of life insurance claims processing
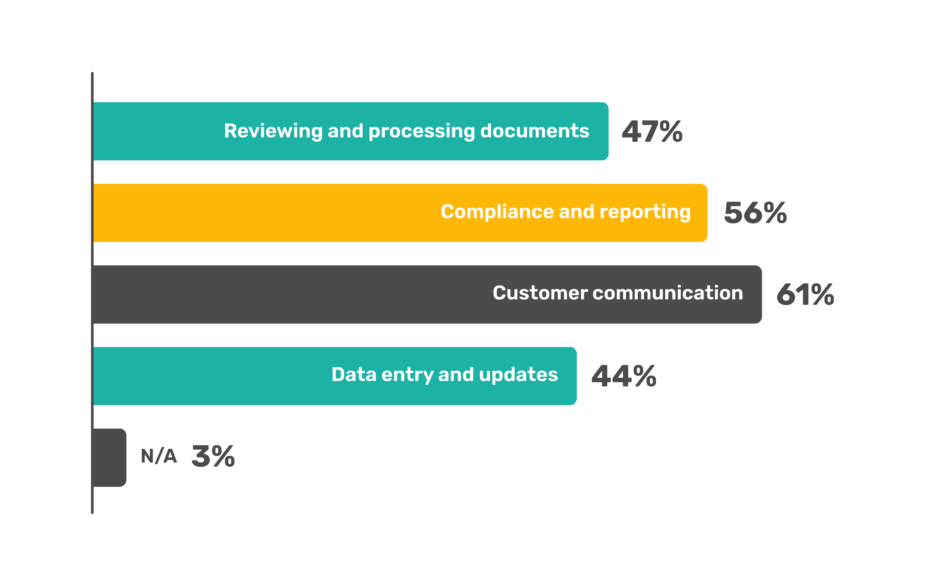
Customer communication
Life insurance claims require high levels customer interaction, often in highly sensitive and emotional circumstances. Our survey revealed that 55% of claims handlers find this particularly challenging.
Reviewing and processing claims documents
51% of respondents find document review and processing to be a major pain point. The nature of life insurance claims means handling various documents, from death certificates to medical reports. Ensuring the accuracy and authenticity of these documents is time-consuming.
Data entry and updates
49% of respondents expressed frustration with data entry. Managing extensive data associated with life insurance claims, including multiple touchpoints and varied documentation, can lead to errors and delays if done manually.
Factors contributing to delays in life insurance claims
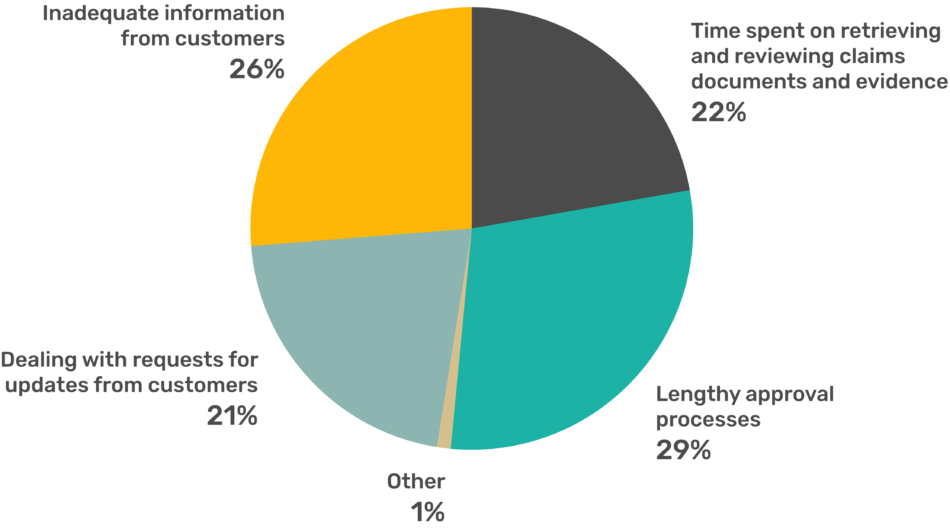
Lengthy approval processes
29% of respondents cited lengthy approval processes as a major delay factor. The complexity of life insurance claims necessitates thorough reviews, leading to slower processing times.
Inadequate information from customers
26% highlighted inadequate information from customers as a significant delay factor. Gathering complete and accurate details can be challenging, especially in sensitive situations.
Time spent on retrieving and reviewing documents
22% of respondents pointed to this as a delay factor. The manual effort involved in retrieving and reviewing diverse documentation significantly contributes to processing times.
Enhancing job satisfaction
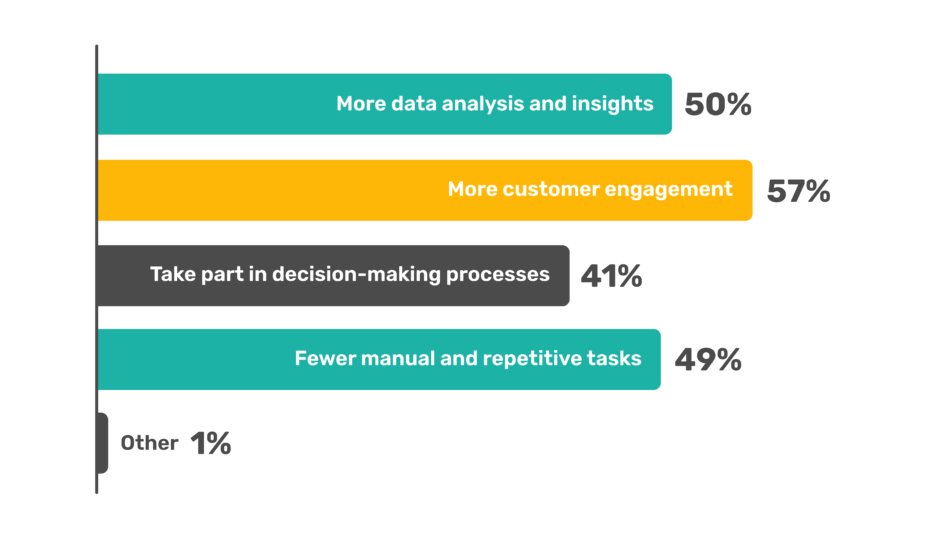
More tools for data analysis and insights
50% of claims handlers believe better data analysis tools would greatly enhance their work.
Fewer manual and repetitive tasks
49% want fewer manual tasks.
Improving customer satisfaction
Faster resolving of claims
34% of respondents believe faster claim resolution is key to improving customer satisfaction.
Automating the claims process
30% see automation as a major improvement area. Implementing automated workflows reduces manual effort, resulting in quicker and more accurate outcomes.
Transparency in the process
20% of respondents noted that customers frequently request more transparency.
Why life insurance claims are suited for automated claims processing
Life insurance claims present unique challenges that make them particularly suited for automated processing.
Automation can enhance efficiency, accuracy, and customer satisfaction by managing complex data and frequent customer interactions, especially during sensitive times. Automated systems can handle routine tasks, allowing claims handlers to focus on providing empathetic support and clear communication to beneficiaries.
Life insurance claims involve a diverse range of documents and data points.
– Claims require the verification of multiple documents like death certificates, medical reports, and beneficiary details.
– Claims handlers interact with customers, medical facilities, and legal representatives.
The benefits of automating life insurance claims processing
– Efficient data handling: Automated systems quickly scan, verify, and process large volumes of documents.
– Error reduction: Automating data entry and validation minimises the risk of human error.
– More time for customer support: By reducing the manual workload, claims handlers can spend more time providing empathetic support and clear communication to customers.
– Clear information from the start: Automation ensures that any missing information is identified and communicated promptly.
– Streamlined workflows: Automated systems streamline approval workflows and track progress in real-time.
– Faster approvals: Automating routine checks and approvals reduces processing time.
– Fewer challenges in information gathering: Incomplete submissions can complicate communication and information gathering.
– Intelligent data extraction: AI can extract and interpret data from documents in various languages.
How Sprout.ai processes life insurance claims
Sprout.ai uses your claim handling philosophy to deliver the best possible outcome for both insurers and customers, achieving 98% accuracy often within seconds. This allows claims handlers to focus on complex claims that require a human touch and high levels of expertise.
1. Claim classification
The claim is initially classified to understand its nature. For example, in the case of a life insurance claim, it might involve incidents such as death benefits, accidental death, or terminal illness benefits. This step sets the stage for detailed investigation and flags any missing information that may be crucial for processing.
2. Cause analysis
The cause of the claim is thoroughly analysed. For instance, if the claim is for a death benefit, the analysis will determine the cause of death to establish liability and understand the context of the incident.
3. Assessment
The severity of the incident is assessed. This includes evaluating the required documents for life insurance claims and the value of the benefit. This step ensures that the claim is accurately quantified and that necessary interventions are identified.
4. Inclusion checking
The claim is then checked for coverage under the customer’s specific life insurance policy. This involves verifying policy details to ensure the incident is covered. Verification can be conducted through a digital policy administration system or by using natural language processing (NLP) to interpret the terms directly from the policy document.
5. Exclusion verification
Potential exclusions are reviewed to ascertain if the claim falls under any policy exclusions. This step is crucial to ensure that claims are not wrongfully processed or denied. Like inclusion checking, this can be achieved via a digital system or through an NLP review of the policy document.
6. Special terms
Any special terms related to the policy are examined. These might include unique inclusions or exclusions that are not typically covered in the standard policy language and are often stored in an unstructured format. This examination ensures all conditions and clauses of the policy are considered and can also be facilitated through digital systems or NLP.
7. Settlement calculation
Finally, the appropriate payment is calculated based on the outcomes of the above steps. Advanced deep learning algorithms can be employed to align the settlement with the insurer’s claims handling philosophy, ensuring accuracy and fairness in the compensation provided. This technology allows claims handlers to allocate more time to complex cases that require detailed attention and expert judgement.
Conclusion
Sprout.ai streamlines life insurance claims processing, ensuring quick, accurate, and fair settlements. By automating routine tasks, Sprout.ai allows claims handlers to focus on more complex aspects of claims and provide better support to customers, improving efficiency and customer satisfaction.
Read about the top challenges for pet and travel claims, and how to solve them too.

